PI-RADS Score Simply Explained – To Biopsy or Not To Biopsy?
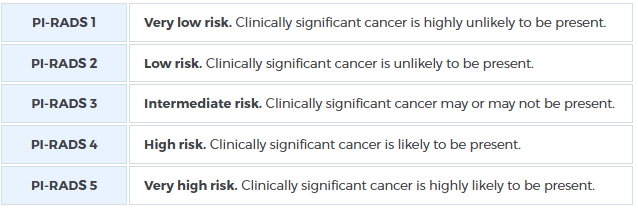
PI-RADS Score is a rating scale for the likelihood that clinically significant prostate cancer (PCa) is present. It is a 5-number system, from least likely to most likely:
A panel of prostate imaging specialists developed the PI-RADS system to improve consistency and agreement among radiologists interpreting prostate MRI scans. The system provides standardized descriptions of which imaging sequences to use and how prostate cancer (PCa) presents in each sequence.
Since its initial release in 2011, the PI-RADS system has undergone two updates. Each new version incorporates advances in both biology and technology, further enhancing diagnostic accuracy. This has been particularly beneficial for experienced radiologists like Dr. Sperling, who specialize in prostate imaging, ensuring even greater precision in interpreting MRI scans.
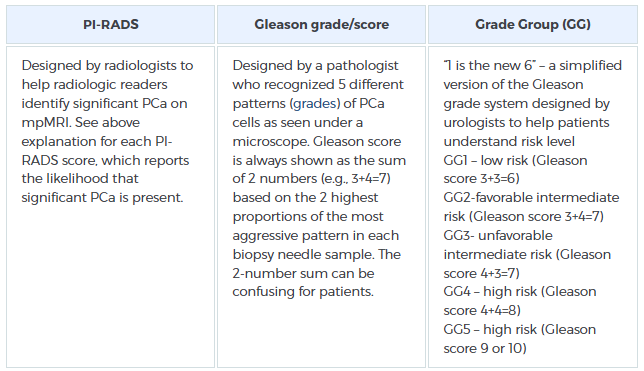
Is PI-RADS the same as Gleason score and Grade Group?
Experts currently use three scales to “rank” the danger of PCa. They are parallel but not identical, since each gives important information in slightly different ways. Compare the slight differences:
The Benefits of PI-RADS
To fully appreciate the benefits of PI-RADS, it’s essential to understand the evolution in prostate cancer (PCa) diagnosis. When experts use a high-powered magnet, mpMRI combined with PI-RADS can improve diagnostic accuracy significantly. While TRUS biopsy can provide valuable information, it comes with significant risks, including infection, bleeding, and pain. Moreover, it has a substantial error margin of at least 30%. TRUS often over-detects insignificant cancer and misses more aggressive cases. This leads to treatment mismatches, unnecessary side effects, and poor outcomes.
Today, men with suspicious PSA results can benefit from a less invasive intermediate step: mpMRI. When experts use a high-powered magnet, mpMRI combined with PI-RADS can improve diagnostic accuracy significantly. The PI-RADS score helps determine whether a biopsy is necessary. For example, doctors usually skip biopsy for PI-RADS scores of 1 or 2. They perform biopsy for scores of 3, 4, or 5. Studies show that with mpMRI and PI-RADS, up to 50% of patients avoid biopsy at the time of the scan.
What if PI-RADS Indicates a Biopsy is Necessary?
If a PI-RADS score suggests a high likelihood of clinically significant prostate cancer, a needle biopsy is essential for an accurate diagnosis. This is because only a biopsy provides actual tissue samples that can be examined under a microscope. If prostate cancer is present, understanding its precise location, shape, size, and aggression level is key to determining the best course of treatment.
At the Sperling Prostate Center, we offer the most advanced biopsy technique available. Once a PI-RADS score indicates the need for a biopsy, our real-time, in-bore MRI-targeted biopsy stands out in several critical areas:
- Precise targeting: The suspicious area is visualized in real time, allowing for highly accurate targeting.
- Minimal needles: Only a small number of needles (usually 2-4) are used to sample the areas most likely to contain the most dangerous cells. This helps guide the planning of the most effective treatment.
- Increased accuracy: Real-time MRI guidance offers superior accuracy compared to fusion-guided biopsies, which rely on pre-captured MRI images and can suffer from alignment errors. Fusion biopsies often require additional systematic needle sampling to compensate for potential misalignment.
By using in-bore MRI-guided targeting, we eliminate the errors inherent in fusion biopsies, offering a more precise and effective diagnostic procedure.