What is Prostatitis?
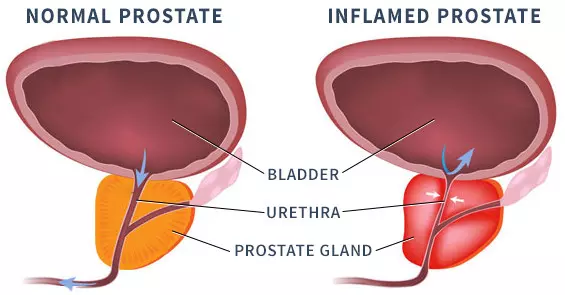
Prostatitis is the inflammation or swelling of the prostate gland. While it can be caused by an infection, standard diagnostic tests often fail to pinpoint a specific organism. This presents a challenge, particularly when the condition is chronic (recurring over time).
Common symptoms of prostatitis include:
- Pain in the pelvic area (genitals or deeper in the groin) or lower back
- Painful or difficult urination
- Sexual dysfunction or painful orgasms
- General health issues such as flu-like symptoms, fatigue, and depression
- Elevated or rising PSA levels
Diagnosis is Challenging
Diagnosing prostatitis can be difficult due to its overlap with other prostate conditions. One common test, a basic urinalysis, misses 85% of the bacterial strains that can cause prostatitis.
In typical practice, doctors begin by gathering a detailed history of symptoms and other related issues. Lab tests may include urine, blood, and prostate fluid analysis, along with a digital rectal exam, which only examines one part of the prostate. A physical urological exam may also be performed. If the results are unclear, a diagnosis of Chronic Pelvic Pain Syndrome (CPPS) is often given, especially if pain or urinary problems have persisted for at least 3 of the previous 6 months. If PSA levels are elevated, a biopsy may be recommended to rule out prostate cancer.
The Four Types of Prostatitis
- Acute Bacterial Prostatitis: This type develops suddenly or gradually due to a bacterial infection. It typically resolves with a full course of the appropriate antibiotics.
- Chronic Bacterial Prostatitis: This condition either persists or recurs in cycles because antibiotics didn’t eliminate all the bacteria. It may be difficult to treat, especially if the bacteria are resistant to drugs.
- Chronic Prostatitis Without Infection: This type shares symptoms with chronic bacterial prostatitis, but no infection is found. It is often difficult to diagnose accurately, and antibiotics are ineffective. Sometimes, this may actually be Chronic Pelvic Pain Syndrome (CPPS), which is caused by tense pelvic floor muscles.
- Asymptomatic Prostatitis: This form has no symptoms but is detected when diagnosing other pelvic health issues. A doctor will determine whether treatment is needed.
What are the Causes?
Prostatitis is commonly caused by a bacterial infection, which requires antibiotic treatment to prevent the condition from worsening. However, symptoms that resemble prostatitis can also result from injuries to the groin area or nervous system issues. When conventional tests fail to identify the specific cause of the infection, the Sperling Prostate Center provides an advanced urine test that can detect organisms that other tests may miss.
I’ve had intermittent lower pelvic pain, which my doctor diagnosed as Prostate Inflammation, but antibiotics didn’t work. Now he says I might have CPPS. What is that?
CPPS stands for Chronic Pelvic Pain Syndrome. While prostatitis is often linked to CPPS, prostatitis may not always be the true cause. CPPS can be more challenging to manage than prostatitis, and the pain may actually stem from nerve irritation caused by pelvic floor tension. However, pinpointing the exact source of nerve pain can be difficult, as it may be referred pain (felt in one area but originating elsewhere). Only a doctor can properly diagnose your situation. It may be helpful to seek a second opinion from a specialist in CPPS in your area.
Is there a better way to determine if it’s a Prostate Inflammation or CPPS?
Symptoms of prostatitis and CPPS can vary greatly between patients. To improve diagnostic accuracy, researchers have created a 6-category system called UPOINT, which helps cover all potential causes. UPOINT is an acronym for the following categories:
- Urinary symptoms
- Psychological dysfunction
- Organ-specific symptoms
- Infectious causes
- Neurologic (nerve) dysfunction
- Tenderness of the pelvic floor muscles
This system assists in the diagnostic process and helps personalize treatment plans. Additionally, we strongly recommend obtaining a baseline multiparametric MRI (mpMRI) as soon as possible to examine the prostate and surrounding tissues. At Sperling Prostate Center, we offer 3T mpMRI – BlueLaser™, which is ideal for screening various prostate conditions. Our advanced imaging technology and expert analysis can detect even subtle changes in tissue that may indicate prostatitis-related inflammation, making it an excellent diagnostic tool for patients with suspected prostatitis.